If you search on the web for the term ‘coronavirus bloodbath’ (which I did after I noticed the term occurring repeatedly in the press), you’ll notice that the headlines are not about the mass deaths of vulnerable people that are inevitable on the sort of bungling business-as-usual trajectory adopted by the likes of President Donald Trump and Prime Minister Boris Johnson.
The headlines are about stocks. Shares. Wall Street. The economy. Oil. Growth. Business. Banks. Finance.
Sections of the media, incumbent political elites, Wall Street and City of London investors are obsessed with the ‘bloodbath’ that is taking down the economy.
But this is not fundamentally an economic crisis. It’s a public health crisis. While global economic growth in its current form is structurally beyond salvage — the lives of human beings at risk from the spread of the novel coronavirus are not.
This piece sets out in stark terms what is at stake. I’ve used the available data and trends to extrapolate a series of ‘business-as-usual’ projections which convey the scale of what could happen without urgent ‘delay’ and ‘mitigation’ efforts being implemented right now. These are not forecasts, but thought-experiments — derived however from reasonably plausible worst-case assumptions — to scope the scale of the risk.
A worst-case scenario could see up to 1.5 million deaths in the UK, and up to 7.6 million deaths in the United States, based on assuming the highest estimated fatality rate. These scenarios are entirely avoidable. I do not believe they will happen at this full-scale: as crisis deepens, it will likely trigger more draconian measures which will have a dampening effect. But the longer that stronger social distancing measures are postponed, the greater the trend toward worst-case outcomes and higher likelihood of more intense (but belated) draconian actions. In this way, my concern is that current US and UK government strategies make higher fatality rates more likely by failing to slow the infection spread and thus rapidly overwhelming healthcare facilities early on.
If you’re reading this, specifically if you’re in a position of power as a national government official, a parliamentarian, a local authority manager, business leader, nonprofit pioneer, entrepreneur, media professional, community leader, headteacher, company manager, or whatever, it’s long past time to get on board for the sake of humanity and life itself.
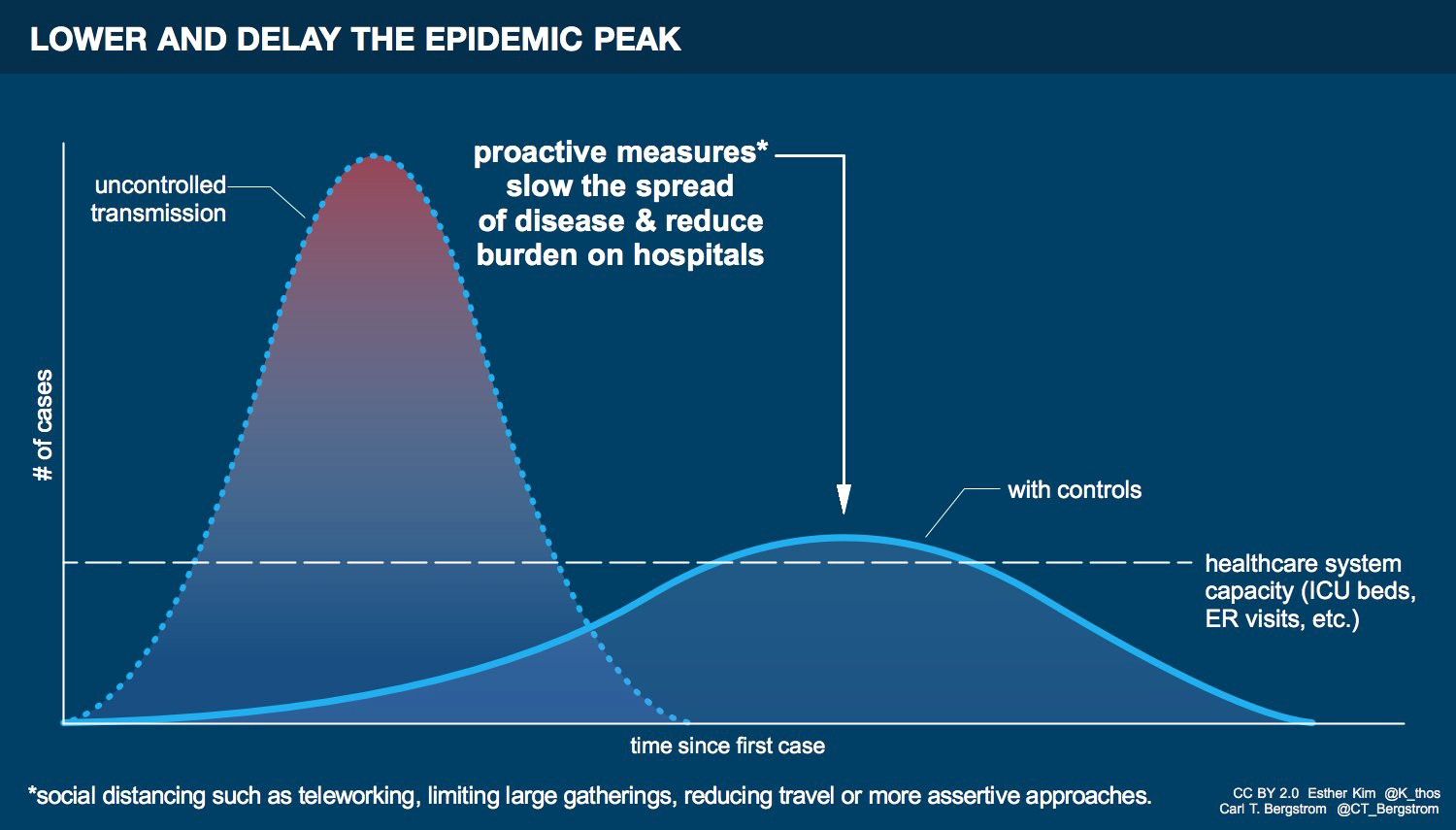
Simple maths and scientific evidence prove unequivocally that without significant early efforts to slow and delay the spread of the virus through radical social distancing, mass deaths become more and more likely the longer such measures are postponed. Further, the only way to minimise the societal dislocation caused by radical social distancing is for the system to shift away from elevating narrow self-interest toward maximum mutual, networked support, particularly for the most vulnerable.
In coming weeks and months, the coronavirus will continue to spread exponentially, will overwhelm national healthcare facilities, and will lead to mass deaths. But it is not yet too late to mitigate these impacts.
Behind the curve
The American and British governments are responsible for flawed decisions which have endangered our populations.
Both have pursued courses of action that have accelerated the spread of infection, making the deaths of many vulnerable elderly and ill people inevitable.
In the United States, President Donald Trump is about to preside over one of the most colossal public health disasters ever.
Not only did the US government’s inexplicably incompetent response end up facilitating the spread of the virus in the homeland, Trump has gone to pains to downplay the risk of the virus — more concerned about maintaining the stock markets. His decision to ban all flights from Europe to the US comes late in the day and will fail to contain the exponential spread of the virus within the US, already well underway.
Whether due to lack of funding or political will in the White House, the Centers for Disease Control failed to manufacture sufficient test kits. As a result, tests are not only unavailable around the country for the growing number of ordinary citizens falling ill, due to the scarcity of test kits healthcare workers who have fallen ill are being denied testing too.
The result is that large numbers of people getting infected with the coronavirus across the United States are not being detected — and the number of official coronavirus confirmations in the US is therefore artificially low.
Across the pond, the British government is failing in a different manner.
During a television interview on 5th March with Philip Schofield and Holly Willoughby on This Morning, Prime Minister Boris Johnson made reference to one ‘theory’ which his government was attempting to balance against other priorities. He explained the theory as follows:
“One of the theories is, that perhaps you could take it on the chin, take it all in one go and allow the disease, as it were, to move through the population, without taking as many draconian measures. I think we need to strike a balance, I think it is very important.”
He went on to say that he did not prefer this theory:
“But I think it would be better if we take all the measures that we can now to stop the peak of the disease being as difficult for the NHS as it might be. I think there are things that we may be able to do.”
But the government’s position has been at odds with itself for months.
Johnson indicated that the government recognises the need to reduce and delay the peak of the epidemic in order to reduce the burden on the National Health Service — and thereby reduce the fatality rate. This is the standard approach recommended by medical experts, grounded in the scientific data. They call it ‘flattening the curve’.
Yet what Johnson also inadvertantly revealed is that someone in his government was bandying about another ‘theory’: the extraordinary notion that the government should do nothing and allow the virus to infect nearly everyone sooner rather than later.
Although the Prime Minister indicated that this was not what he believed to be the “better” option, this isn’t a real scientific theory at all. It has no foundation in medical science, and is unsupported by the data. But someone in his government has debated this theory.
While Johnson said that he wanted to pursue measures that would reduce the burden on the NHS, the government had still refused for a whole month to move out of the containment phase (tracking infected people and who they could have potentially infected and moving them into self-isolation or quarantine) into the ‘delay’ phase which would implement more stringent social distancing measures necessary to do so.
Yet the failure of this approach is unmistakable. On 11th March, UK Health Minister Nadine Dorries tested positive for coronavirus. The government had no idea how she became infected. She had met and potentially put at risk hundreds of people, including Cabinet officials and other members of Parliament. The implication is undeniable: the spread of this novel coronavirus is out of control to the point that a senior government minister is infected and the authorities are incapable of identifying how this happened.
Nadine Dorries is stark proof that the coronavirus is well on the way to becoming endemic. This is the direct result of the government’s irresponsible decision to postpone meaningful delay actions through social distancing for several weeks.
The question, then, is who inside Boris Johnson’s government promulgated the ‘theory’ of allowing the virus to ripple through the population?
According to ITV’s Robert Peston, this is the active strategy of the British government, which prefers not to slow down the spread of the virus too efficiently, but only at a ‘much delayed’ speed. Specifically, Peston reports that the strategy is the brainchild of Boris Johnson, Dominic Cummings and Matt Hancock:
“The strategy of the British government in minimising the impact of Covid-19 is to allow the virus to pass through the entire population so that we acquire herd immunity, but at a much delayed speed so that those who suffer the most acute symptoms are able to receive the medical support they need, and such that the health service is not overwhelmed and crushed by the sheer number of cases it has to treat at any one time.”
Peston says that the government is reluctant to implement large-scale, systematic, top-down social distancing measures, but to focus instead on guidance for individual behavioural changes.
This approach is premised on the idea that since the spread of the virus is unstoppable around the world, it poses an indefinite ever-present threat to the UK, and that as soon as any restrictions are lifted the virus will simply resurface. Peston’s account suggests that the government has made up its mind — since coronavirus is here to stay, rather than slowing it down too much, we should slow it down a bit, but otherwise allow it to pass through the population to do what needs to be done.
As Ed Yong has reported for The Atlantic, it turns out that ‘herd immunity’ was not necessarily the ‘goal’ of the UK government as such — but that the government’s advisors believed that as the outbreak would in the longer term be uncontrollable, achieving ‘herd immunity’ could be a potential side-effect of large numbers of Britons being infected. This could explain why the UK government did not choose to act earlier — and it now turns out that the scientific modelling used to justify not pursuing early social distancing measures was wrong and will “likely result in hundreds of thousands of deaths.”

Either way, then, the UK government approach simply did not follow automatically from the science. It was based on a particular political interpretation of the science. For instance, Peston claims that the reason for not closing schools is that it would reduce manpower at hospitals and care homes, making them vulnerable to failure. But as we see below, this overlooks the definitive science proving that drastic measures like school closures can prevent the healthcare system from being overwhelmed by dramatically slowing the spread of the virus in the first place.’
Perhaps the biggest hole in the ‘herd immunity’ aspiration is that in order for it to work, a vast majority of the population would need to acquire the virus and become immune to it — but there is no decisive scientific evidence yet that acquiring the virus leads to immunity. Although some scientists see eventual herd immunity as likely, no one knows how long immunity will last, whether it would be permanent, or last only for a few months. Cases of the reinfection of recovered patients have been confirmed in Japan and China. Zhan Qingyuan, director of pneumonia prevention and treatment at the China-Japan Friendship Hospital, warned in a briefing on 31st January: “For those patients who have been cured, there is a likelihood of a relapse. The antibody will be generated; however, in certain individuals, the antibody cannot last that long.”
Take Sir Patrick Vallance’s belief that some after 60 percent of Britons would be infected with coronavirus, this could create ‘herd immunity’, and compare them with this sobering observation from Prof Samuel McConkey, deputy dean at the Royal College of Surgeons in Ireland. He told the Irish Times that he “already expected that [Covid-19] would reinfect people because that is what happens with the previous coronaviruses”.
“The worry is that Covid-19 could spread around the world in a devastating way in March, April and May, and then three months later it could spread around the world again because we are not protected by immunity after the first infection. That’s the worry, that if there’s no acquired immunity it will circulate around for years or until we find a technology to control it.”
This means that based on the current scientific evidence, it is entirely possible that people people do not develop permanent natural immunity. In this case, the only prospect for herd immunity would be for a vaccine to be developed and for the majority of the population to become inoculated which won’t happen for another year to 18 months:
The reality is that without more comprehensive social distancing policies in place as early as possible, the fatality rate will be dramatically higher. By refusing to shift to such measures, the government guarantees higher death rates.
This has now been corroborated by the publication of a report by Imperial College COVID-19 Response Team — which is advising the UK government — which concludes that the previous UK ‘mitigation’ strategy which has avoided wider social distancing policies would “likely result in hundreds of thousands of deaths and health systems (most notably intensive care units) being overwhelmed many times over”. Amazingly, despite warnings from countless experts and scientists, this conclusion was “only reached in the last few days”, says the report.
A projected worst-case scenario for Britain
All the data indicates very clearly that during the period in which governments refused to move to the ‘delay’ phase, the coronavirus has been circulating rapidly across communities in the US, UK and Europe, and is on track for exponential growth.
The British government’s planning for a worst-case scenario appears to severely underestimate the potential risk.
As I show below, the application of this ‘theory’ would lead to something like 70 percent of the British population becoming rapidly infected, potentially leading to the deaths of between 400,000 and 1.5 million people — most of them elderly and ill.
This and the other projections discussed below are not forecasts, but worst-case projections based on do-nothing scenarios derived from very specific assumptions to illustrate the severe risks of inaction. Running through the thought-experiments of these scenarios throws light on what could happen and how difficult it will be to avoid.
The government’s announcement of mild new social distancing measures may mildy mitigate such worst-case scenarios but they come too little, too late. By postponing these and more extensive measures, the government has guaranteed that they will be less effective, and has increased the early burden on the NHS — which will lead to a greater number of deaths that could have been avoided.
We can begin by collating data on the number of confirmed cases in the UK. Below is a graph based on the number of daily confirmed cases of coronavirus in the UK up to 11th March:
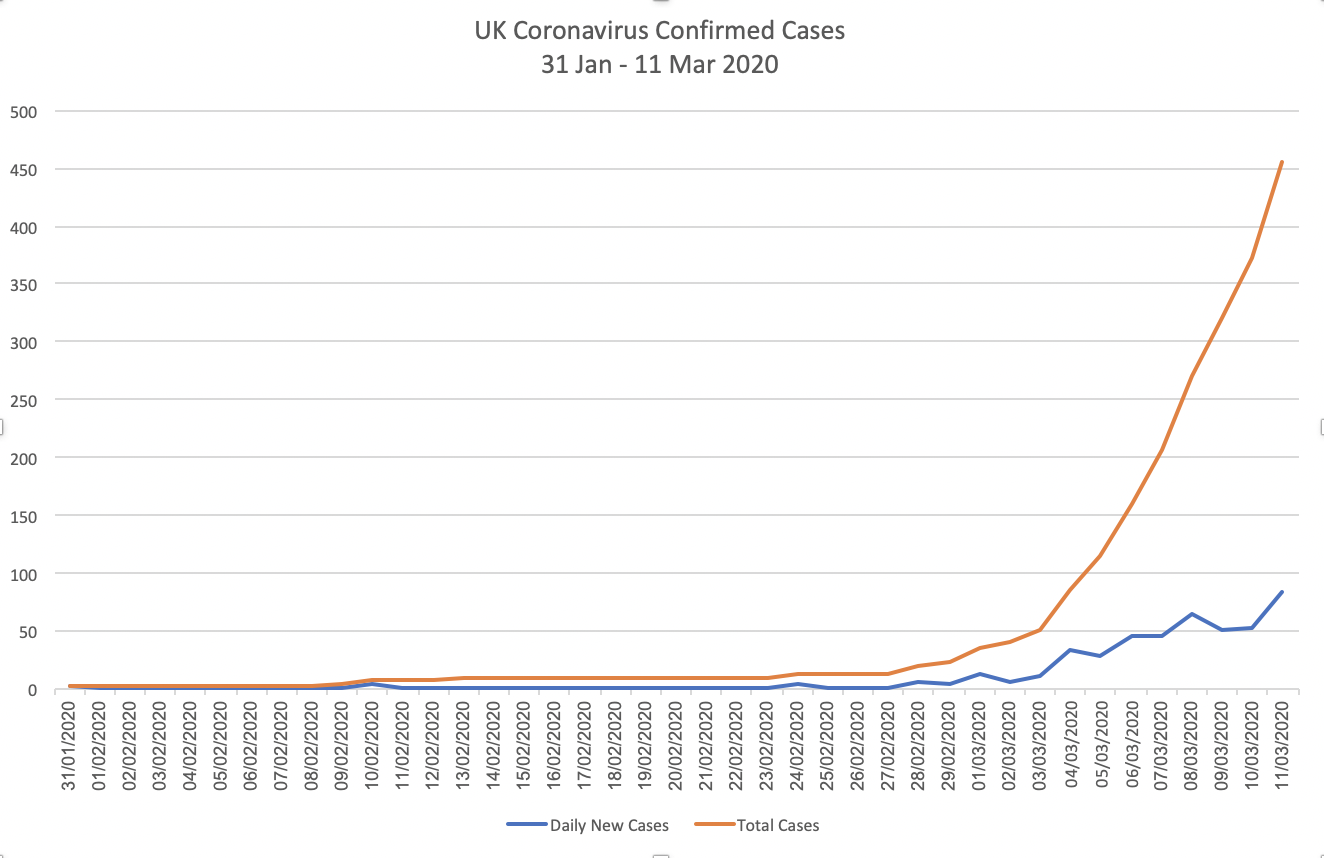
The vertical axis indicates the number of cases. The blue line indicates the number of new confirmed each day, while the red line plots the cumulative total number of confirmed cases overall.
As you can see, as Britain has been rolling out test-kits around the country, we have only begun to catch-up with the number of cases that exist. The number of new confirmed cases coming in each day (blue) is on a fluctuating upward trend. But the red line is the one that’s key — it shows that the number of confirmed coronavirus cases is growing exponentially.
On average, it has been doubling every 2–3 days. UPDATE: As of 13th March, this projected exponential trajectory has been corroborated by the fact that the new confirmed cases have more than doubled over that 2–3 day period.
The underlying reason cases are growing exponentially is simple — it’s due to the basic reproduction number (RO), which indicates how many people a single infected person infects. The available data is still evolving, but so far it shows that the RO is at least 2 and potentially higher depending on the context (different conditions appear to decrease or increase the risk of infection).
In order to explore what we can expect if the current rate of growth in daily confirmed coronavirus cases in the UK continues in this way, I applied the same rate of growth to these numbers and projected it forward. It produces this:
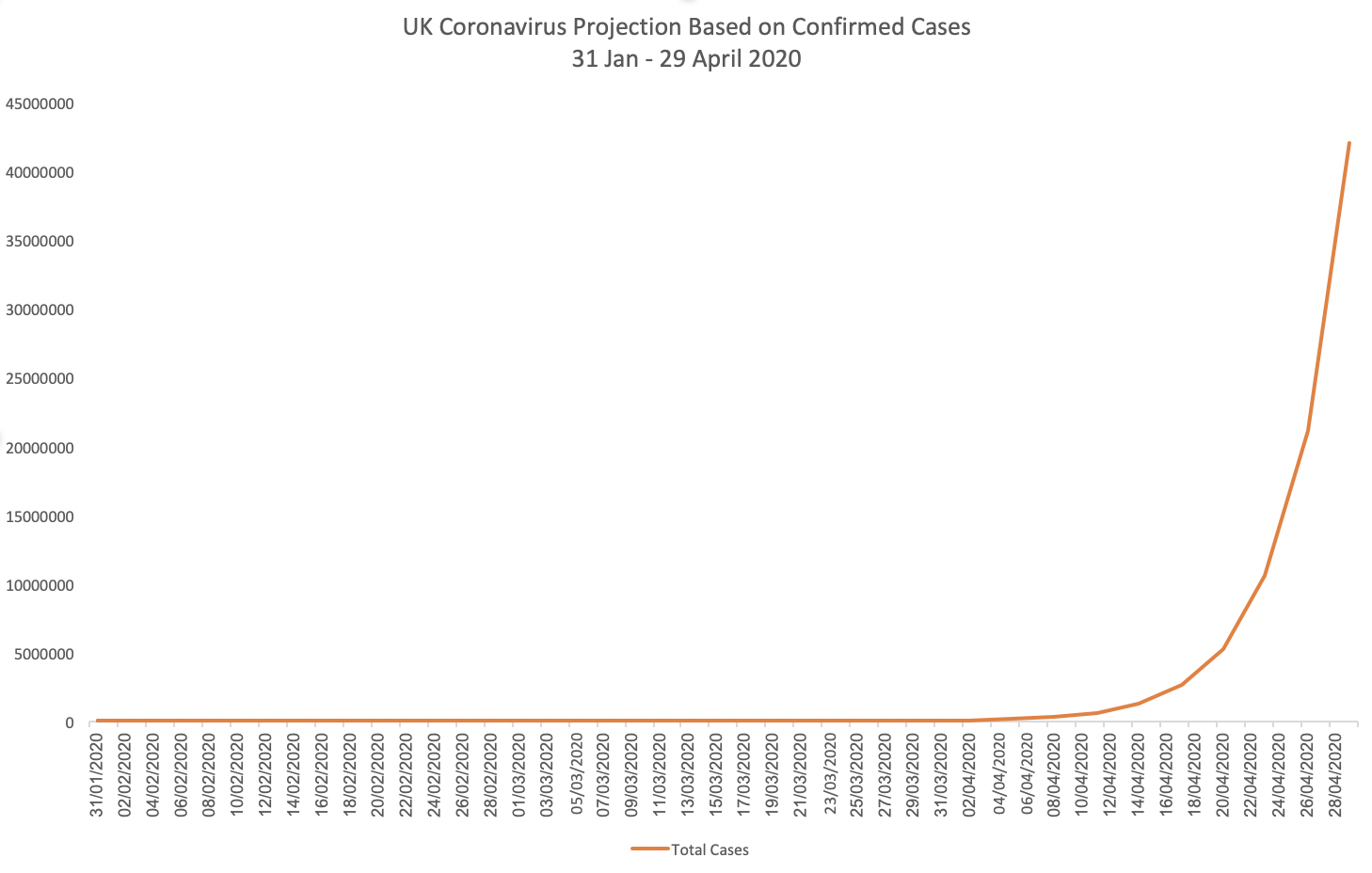
This corroborates what we have already heard from government officials, that the cases will “start to peak” in April. This scenario assumes that no or minimal delay or mitigation efforts are put in place. It shows that under that scenario, the infection rate accelerates around mid-to-late April and continues through to the end of that month at which point, given that rate of growth, a total of 42,074,112 Britons would be infected: some 64 percent of the entire UK population.
The government’s belated new measures will mitigate slightly against a worst-case outcome. But to a significant extent, some of this exponential growth in spread is now locked in due to the failure to move earlier to stronger social distancing measures.
This particular scenario is already devastating, but it might also be a conservative scenario — because the true number of infected people is many multiples higher than the number of confirmed cases.
One way of extrapolating how many multiples — again conservatively — is the case of Washington state, where epidemiologists estimated that the number of infected people was at least ten times higher than the number of confirmed cases at that time, at the end of February. Elsewhere, this ratio is twice if not three times as high. But using that very conservative baseline, we can generate some plausible conservative estimates of the minimum number of infected people in the UK.
Now if we take those estimates and project them forward using the RO of 2 (so each of those infected people would infect two more — once again keeping it conservative), the projected scenario is much faster.
Epidemiological studies based on confirmed cases indicate a doubling rate every six days. But this is an artifact of the extent to which a virus’s spread is tracked by authorities. As Tomas Peuyo has shown, the true number of cases growing is actually much faster than confirmed cases.
Therefore, for this thought-experiment projection I’ve assumed that over a period of 6 days — based on the RO of 2 and an estimated average 5-day incubation period — each of those individuals would be able to infect two more, with each of those infecting two more. This of course also assumes no, minimal, or ineffective social distancing measures.
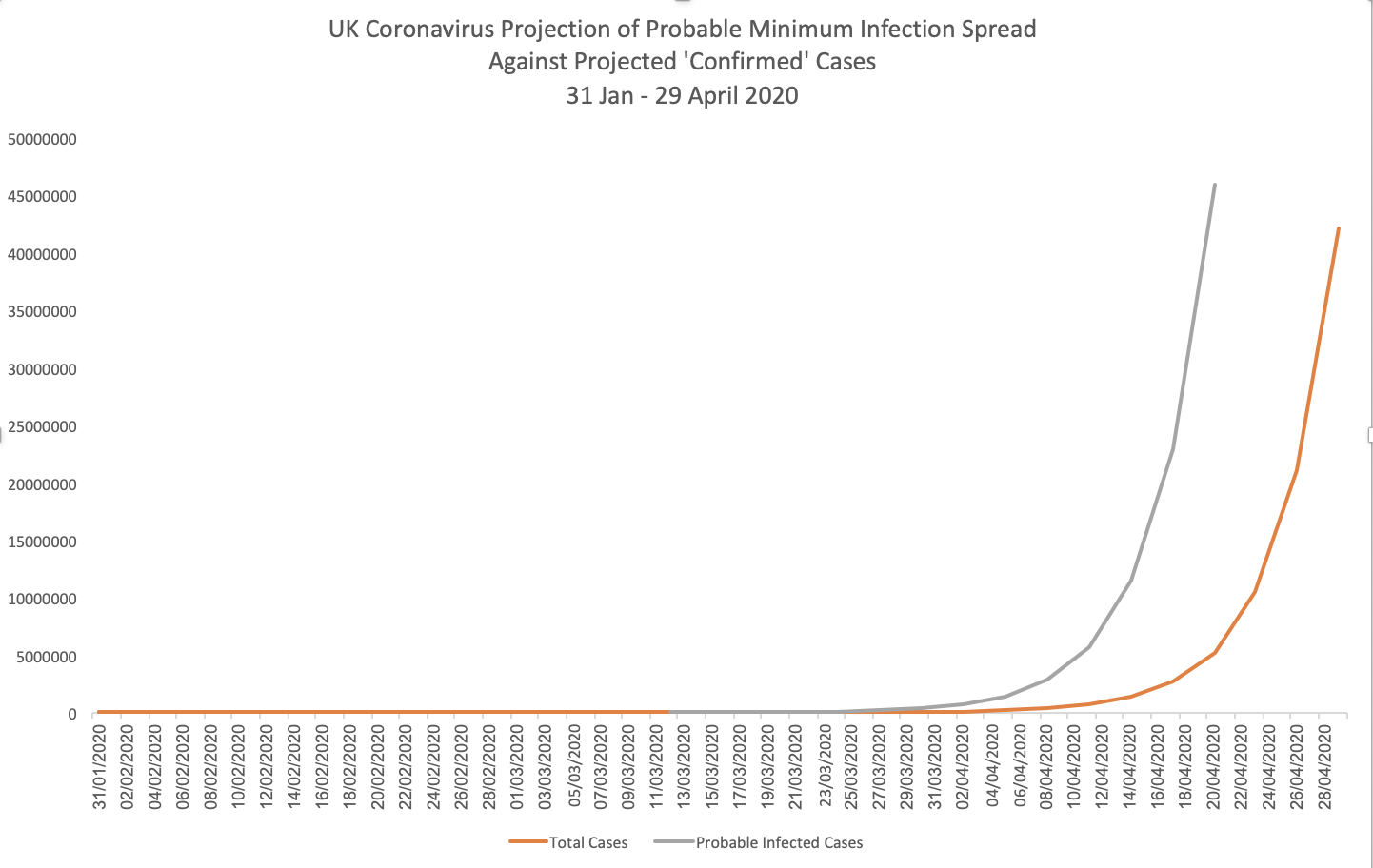
The grey line indicates the estimated minimum number of people probably infected, as compared to the red line indicating confirmed cases. The gap between the two widens, as the actual number of infections spreads, with confirmed cases tracking well below the real epidemic.
The graph indicates that the number of people who may actually get infected in a no-mitigation scenario could reach 45,875,200 people as early as 18th April, 69 percent of the entire population.
How many deaths might we then see in this scenario? There is a best and worst case, based solely on the estimated fatality rate, which could be as low as about 1 percent (still 10 times worse than the common flu); and potentially as high as 3.4 per cent, the figure touted by the World Health Organisation looking at global cases. In reality, this rate would be variable according to the local and national context, healthcare systems, social stratification and many other factors (see UPDATE note two paragraphs below for further discussion of the fatality rate).
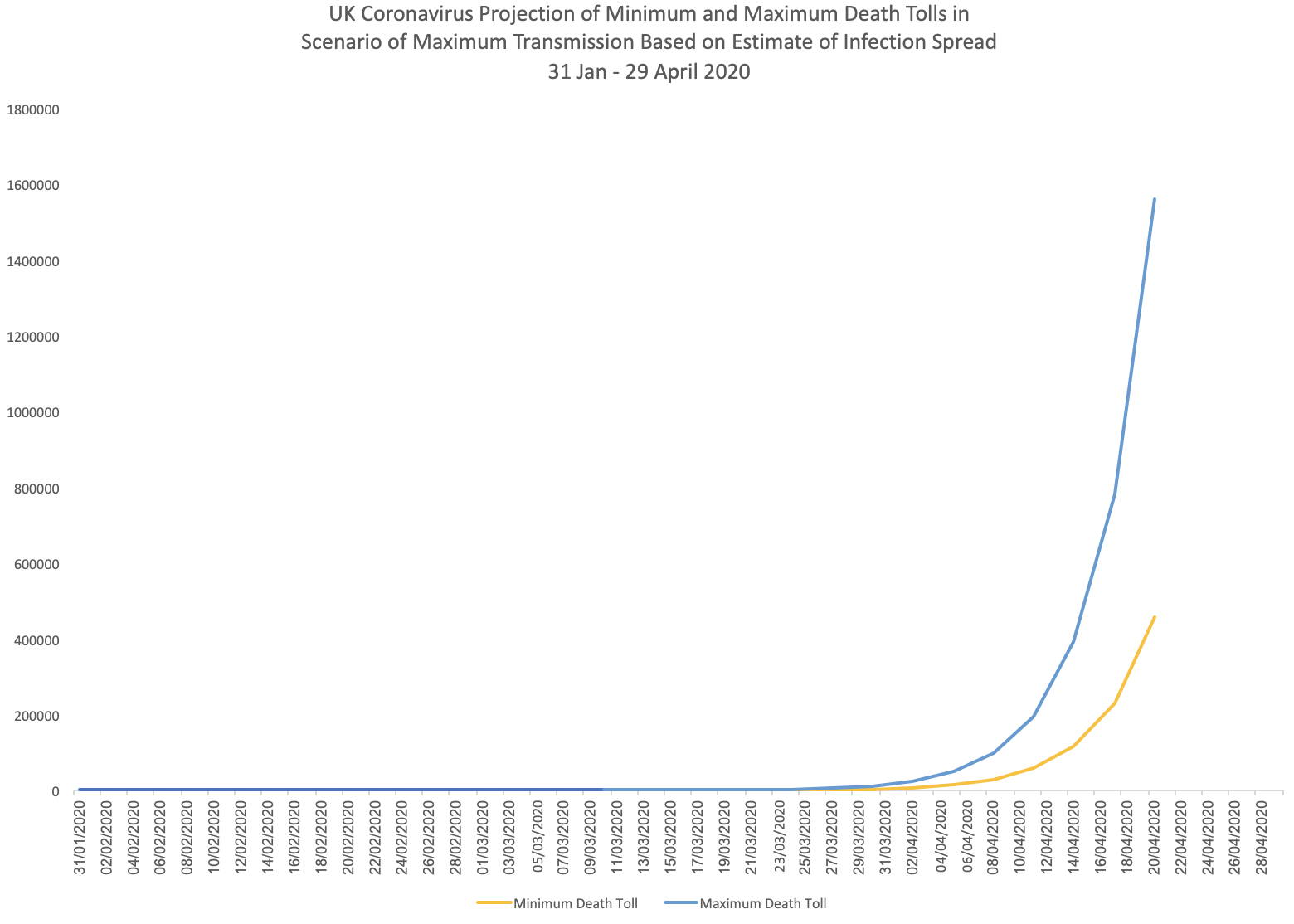
Under this absolute worst-case scenario we’d see a minimum of 458,752 deaths, and a maximum of 1,559,757 deaths. This is because, without comprehensive social distancing measures to slow the spread, the rising number of cases would rapidly overwhelm healthcare facilities as is happening in Italy.
Epidemiologists and virologists largely agree that this scale of death is a plausible worst-case scenario. Dr Jeremy Rossman, Honorary Senior Lecturer in Virology at the University of Kent, has argued that the UK government’s ‘herd immunity’ strategy “could result in the deaths of more than a million people with a further eight million severe infections requiring critical care.”
UPDATE: There has been some speculation that since the infection rate appears to be much higher than we are able to track — several multiples higher, then the mortality rate must be lower than 1 percent, meaning that in reality well over 99 percent of people will be fine. This appears to be the thinking of UK government Chief Medical Officer Dr Chris Whitty.
Yet my concern is that while this is certainly not entirely wrong, it may potentially be misleading because it does not fully take into account the social structural context of variation in fatality rates. When Dr Whitty points out that the 1–3.4 percent range figure is not really accurate, he is right; but to use this as a basis to say the overall fatality rate is likely to be overall lower than 1 percent and therefore this is less worrying, is in my view highly speculative and not yet justified by the available scientific data.
For instance, in Italy the death rate has turned out so far to be extraordinarily high — 6 percent. How do we make sense of this? The 1–3.4 percent range are median figures. To this extent we know they are only indicative, because they provide a median between highly variable fatality rates for different age ranges and health vulnerabilities. The data so far suggests that while people below the age of fifty are highly unlikely to die from coronavirus, the probability of death becomes much higher above that age, and for specific illnesses.
In Italy specifically, the data suggests that the median death rate has rocketed up because of the escalating collapse of the country’s healthcare system — so as more vulnerable people older and already ill people cannot receive sufficient healthcare, their death rate is driven up.
At Italy’s higher 6 percent range, even if many multiples more people in Italy are infected but not at risk of death (implying that the overall median fatality rate would be lower), this would not necessarily bring the overall median percentage all the way back down to below 1 percent: This means that the crucial issue is ensuring that those who end up needing hospitalisation receive the specialized support which allows them to recover. If they don’t, in an overburdened healthcare system, fatality rate can be much higher than the global average percentage.
In short, the fatality figures are still variable and will become more fine tuned as more data comes in. But there is little firm scientific evidence to justify assuming the lowest possible fatality rate on our current course.
With mild social distancing measures in place, we can expect that a worst-case scenario would only be mitigated minimally as the virus continues to spread, including to elderly people when they meet members of their family who continue to mingle as normal (the UK government’s proposed self-isolation period is only 7 days, when the virus can be contagious for longer than 14 days). But even here we can’t be sure of whether even minimal mitigation would happen, due to the fact that the some of the assumptions underlying these projections are conservative.
These projections demonstrate that what the government has told the public about the risk is simply false. Government officials have claimed that a worst-case scenario of 80 percent of Britons getting infected would see around 100,000 deaths. This is the figure against which the government says it is planning with local authorities. The projections above indicate that this estimate is not at all supported by the data.
In reality, based on the estimated fatality rate, the government’s alleged worst-case scenario would require that the infection spread peaks at just around 10 million people — less than a sixth of the population — and assuming the minimum 1 percent fatality rate. So if this is indeed the government’s worst-case planning scenario, the only way to achieve it would be to have the infection peak at a level several orders lower. Meanwhile, the government is deliberately avoiding taking any social distancing measures that might actually facilitate such a low peak.
In short, the government’s worst-case planning scenario is fundamentally at odds with the available scientific data.
Based on the projections above, it appears to be unlikely that the UK government’s new mild delay measures are sufficient to, and will have come in place in time to, dramatically slow the spread of the infection so that it peaks at the government’s own worst-case scenario of only 100,000 deaths — especially given that the projections above suggest that the 10 million mark would be reached by around 12th April.
In short, the next month is absolutely crucial. This is the month in which we need to reduce the spread of infection to as low as possible to minimise fatalities, well below 10 million. This can only be achieved by radical and comprehensive social distancing measures. Our current trajectory is trending toward breaching this several times over.
There are other reasons for concern. While the new, belated social distancing measures might begin to slow the kind of rapid exponential spread indicated in these charts, there are other crucial factors suggesting that a rapid exponential spread is still probable due to the extent of the undetected spread and the long delay in shifting to the delay phase — and because the numbers relied on in these projections are deeply conservative. These factors include:
- The estimated infection spread relative to the number of confirmed cases is too low. I’ve used a factor 10, when that factor is probably higher, meaning that my starting assumptions of probable infection spread early on are likely to be too low. This would mean the real infection spread is already much higher than the confirmed cases, and we just haven’t realised it yet.
- The RO, how many people a single person infects, could be higher than I’ve estimated. The most conservative estimate is 2, but a wide range of emerging data suggests it could be as high as 4 in various circumstances — and one alarming study by Chinese government scientists revealed that a bus passenger was able to infect seven fellow travellers over a 4-hour bus ride, including people who were 4.5 metres away. The study suggested that the virus could linger in the air for up to 30 minutes and remain on surfaces for 2–3 days (this study was retracted without explanation the day after it was covered by the international press, and neither the journal nor the study authors have offered any explanation for the retraction). The bottom line is that there is compelling evidence that the RO is higher than 2.
- When you combine these factors with the problem that some people might be spreading the virus despite being asymptomatic — and that even if they have symptoms they may not realise they have contracted the coronavirus, going on to unwittingly infect others — the result is that if applied to these figures, the actual spread of infection could be much higher and faster than projected here. In that case, the government’s belated social distancing measures would not be sufficient to slow down this spread, and we may continue to see a rapid, exponential increase of a similar scale.
A projected worst-case scenario for the US
Just as Boris Johnson’s new measures — while better than nothing — come too little, too late, so too does Trump’s ban on European flights.
Public health officials across the United States have confirmed that the coronavirus is beyond containment. As most states, even those declaring states of emergency, have failed to move rapidly to ‘delay’ measures, this has allowed exponential spread to accelerate. We will see the dire results of this in time.
We can project how fast this will happen in the US in a similar fashion to above.
Let’s take the estimates for the number of undetected infected people in Washington state at the beginning of March. As noted above, the most probable conservative range was around 300–500 people, more likely around 1,100. In the Bay Area, Peuyo estimates 600 cases.
So let’s work with those very conservative figures for the total number of infected in the US as of early March: 1700.
Remembering that the true figures as the epidemic spreads through multiple states simultaneously will be much higher, just projecting forward this number alone produces the following result:
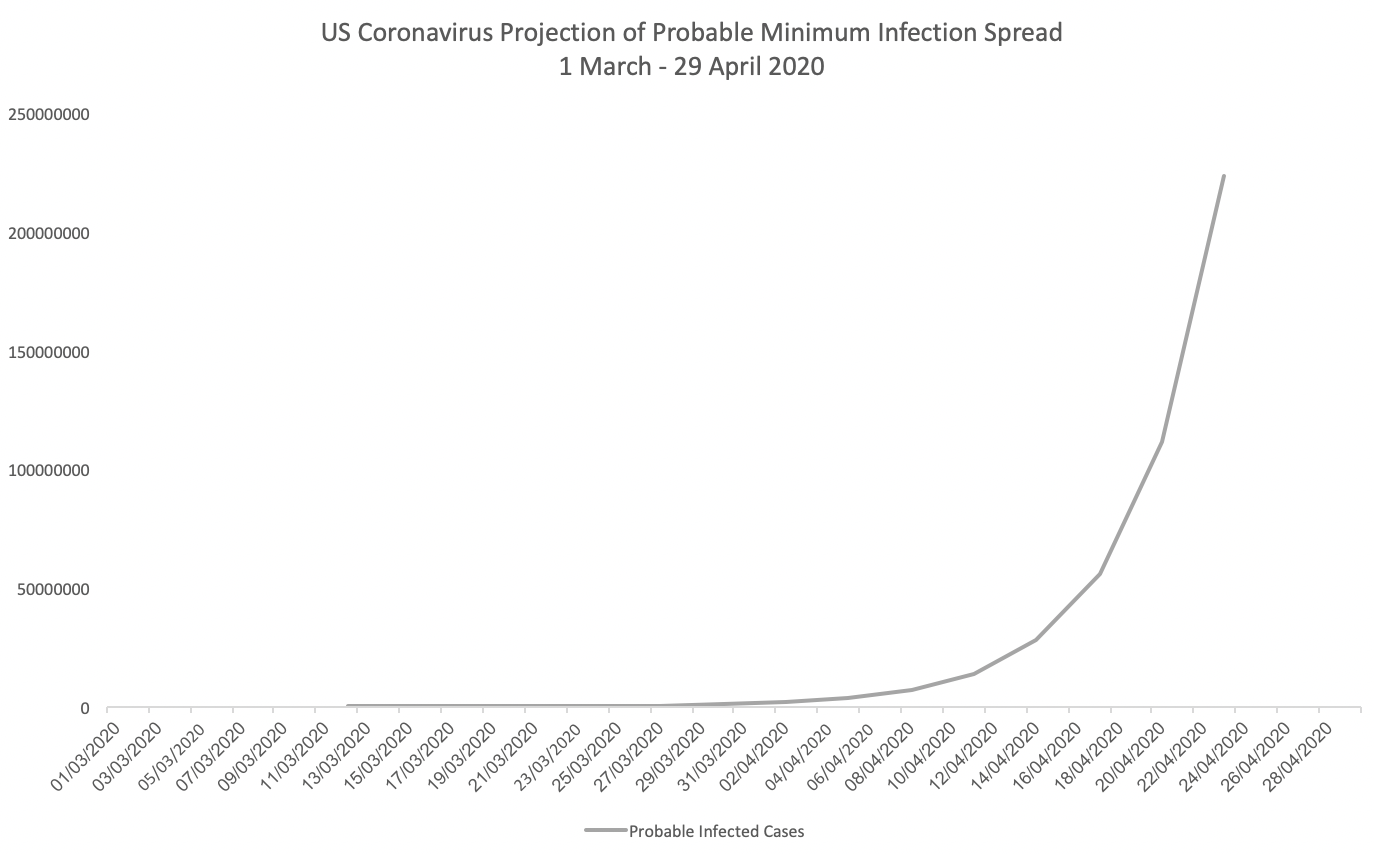
Under this business-as-usual scenario, based on our pessimistic but reasonably plausible infection rate assumptions, the US could see 222,822,400 Americans infected as early as 26th April — some 68 percent of the entire population. One could either see this extending forward in time due to a longer and slower infection rate, or speeding up given that the actual number of undetected infections that currently exist across the US are likely to be several orders higher than the figures used here.
Given a 1 percent fatality rate, approximately 2,228,224 Americans would die in this scenario. Given a 3.4 percent fatality rate, approximately 7,575,962 Americans would die in this scenario.
As with the UK projections, there are many reasons to suspect that some of the assumptions behind the US scenario are too pessimistic (the rate of infection spreading for instance). A slower infection spread in the real-world would create more lead-time for action and greater opportunity to lower mortality rates.
On the other hand, the starting figures are almost certainly way too small, with the numbers of infected in the US probably well into their thousands. With containment efforts having already failed, few social distancing measures in place, and the RO potentially higher than 2, this could suggest that the scenario above is actually closer to reality.
Now what? Community solidarity in slowing the virus
At this point, these projections make one thing very clear: we cannot afford to wait around debating the speed and slowness of what is most definitely not just coming, but already here. We are already too late in acting. But it’s not too late to drastically mitigate the public health catastrophe that is now bound to erupt in coming weeks.
This means that the imperative right now is for people in all sectors of society to pull together, work together and help each other in implementing radical action aimed at slowing and preventing the spread of the virus; while implementing policies to protect the most vulnerable in our societies, particularly the poor, the homeless, the elderly and the ill.
Contrary to the claims of US and UK government officials, scientific studies prove clearly that only radical social distancing can save lives.
Over ten years ago, a landmark study in the Proceedings of the National Academy of Sciences examined the effectiveness of early social distancing interventions during the 1918 Spanish flu epidemic in the US. The study showed that radical actions executed early on were able to reduce peak death rates by as much as 50 percent.

The study looked at 17 different American cities, and the timing of 19 different types of intervention. It found:
“… cities in which multiple interventions were implemented at an early phase of the epidemic had peak death rates ≈50% lower than those that did not and had less-steep epidemic curves. Cities in which multiple interventions were implemented at an early phase of the epidemic also showed a trend toward lower cumulative excess mortality, but the difference was smaller (≈20%) and less statistically significant than that for peak death rates.”
In this scenario, most cities implemented major social distancing policies such as school closures, bans of large gatherings and so on, for no longer than 6 weeks.
The peer-reviewed study also noted that viral spread would indeed be renewed when such measures are relaxed. But the point is not to eliminate the spread of the virus: that’s now impossible. By delaying its spread, we can mitigate the impacts, make them more manageable, keep our healthcare facilities functional, and save far more lives.
A more recent 2014 peer-reviewed study in PLOS ONE, which modelled the effects of school closures in hypothetical flu epidemics, found that depending on the assumptions, school closures “can lead to reductions of 20–60% in the peak incidence of an epidemic and smaller (0–40%) reductions in the size of the epidemic.”
The UK government approach, in contrast, is topsy-turvey — ‘allow the virus to pass through the population by maintaining schools and big football matches, in order to keep hospitals fully manned’. The data above shows that the government’s refusal to adopt measures like school closures will fail to protect lives, rapidly overwhelm health-systems and drive much higher fatality rates.
There is also emerging science indicating that curtailing public transport can be hugely effective in stopping the spread of the virus.
A team of US, British and Chinese scientists found that the most effective measures that stemmed the spread of the virus across the Chinese mainland included the suspension of intra-city public transport, closing entertainment venues, and banning public gatherings.
The study chimes with other data demonstrating the instrumental role that public transport appears to have played in China in transmitting the virus within and between cities. That paper concluded that there was a “strong and significant association between travel by train and the number of 2019- nCoV cases.”
So when officials claim that there is ‘no science’ for how taking large-scale systematic social distancing measures can hugely mitigate the virus, they are simply wrong.
And the danger is that if we do not move collectively to wider social distancing measures urgently, we will be forced into doing so in a far more draconian way down the line, in the same way that Italy has had to.
This, in fact, is now exactly what has happened since this article was first authored — the Imperial College COVID19 Response Team advising the UK government has had to recommend an urgent “epidemic suppression” strategy with dire social and economic consequences to attempt to make-up for this lost time. Under the government’s previous strategy, the Imperial College report warned that “the surge limits for both general ward and ICU beds would be exceeded by at least 8-fold under the more optimistic scenario for critical care requirements.” Even in a best-case scenario under the old strategy of all patients receiving treatment, the models projected some 250,000 deaths in the UK. In the US, the Imperial College team estimated a best-case of some 1.1–1.2 million deaths under the old strategy.
Despite the turnaround in policy now being pursued, the damage has been done and we have lost valuable time. We are therefore very likely to be on track for preventable catastrophe. While we can now hope that the highest level figures can be avoided, many deaths will now take place that did not need to.
The disaster has already begun to unfold. As confirmed coronavirus cases surge beyond the UK government’s expectations, I have received messages relaying concerns of a doctor at UCL Hospital in Bloomsbury, London, who is the friend of a mutual third party. The messages from that party describe a phone call with the doctor. The messages were sent on Friday March 13th.
Although I have not been able to speak directly with the doctor I have independently verified the authenticity this account.
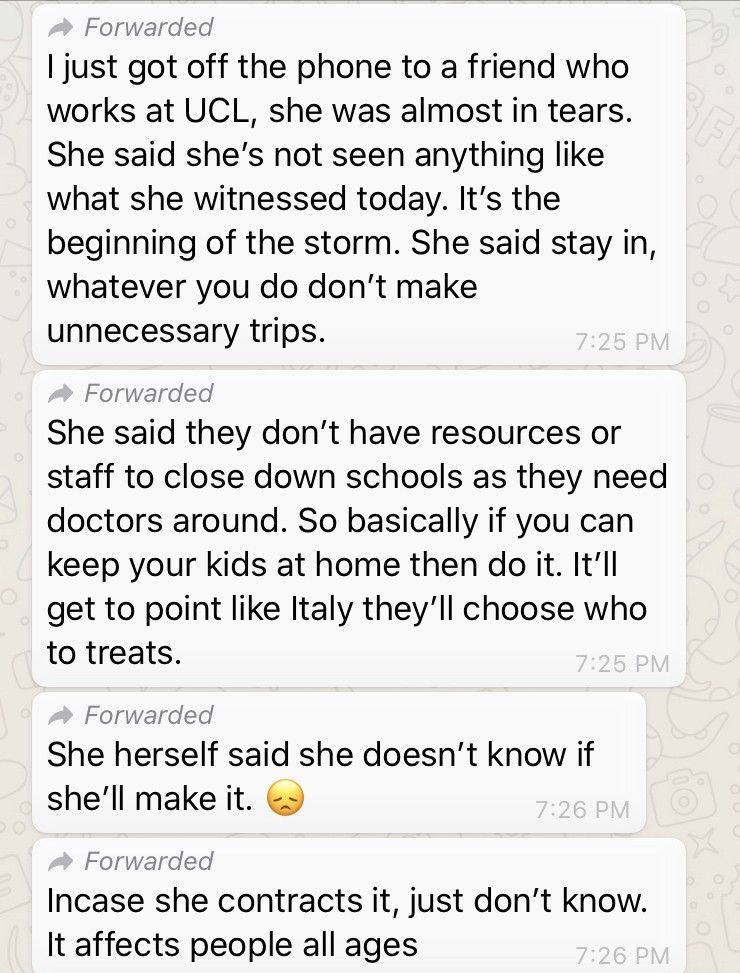
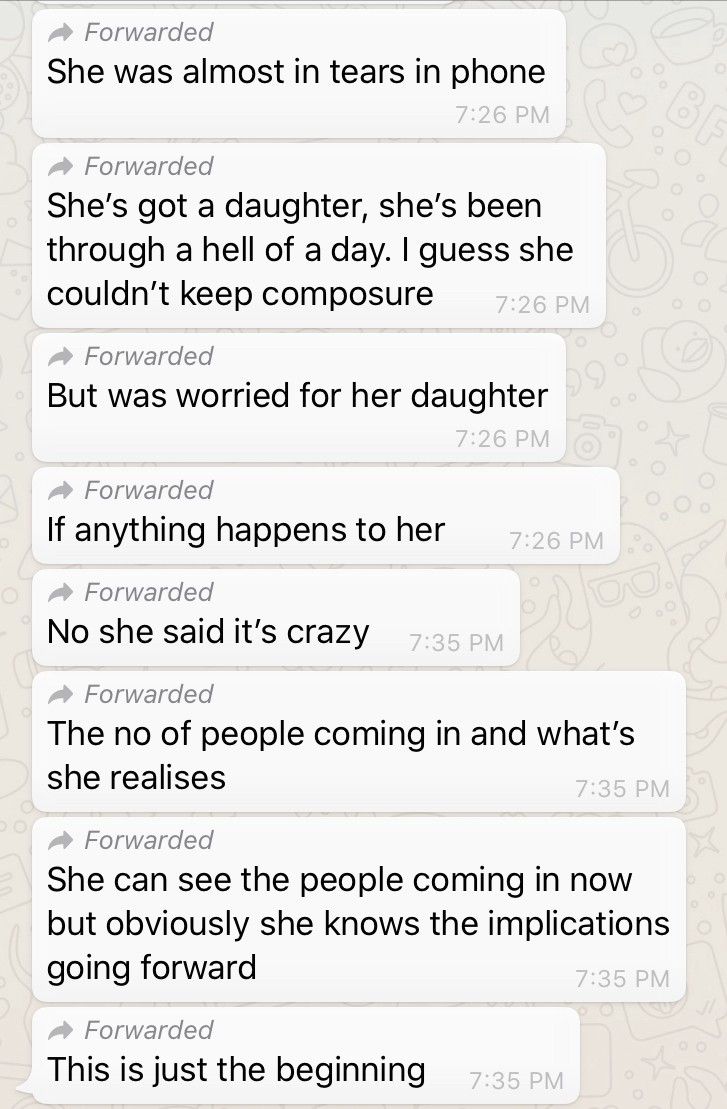
According to the messages, UCL hospital is already becoming overwhelmed with cases relating to coronavirus. The doctor “has not seen anything like what she witnessed today. It’s the beginning of the storm.” The message refers to the “no of people coming in” and asserts “This is just the beginning.”
The messages suggest that one reason the UK Govt may not be keen to close down schools due to ‘timing’ is not because it is still too early, but because we have past that point — and there is an anticipation that the window of opportunity to prevent the NHS from being overwhelmed is long past:
“… they don’t have resources or staff to close down schools as they need doctors around… It’ll get to point like Italy they’ll choose who to treats.”
The doctor apparently privately fears for their own life believing it likely that they will become infected, and is worried about the prospects for her own daughter.
The shift
So whether it comes via government advice or decree, or through businesses and local authorities taking their own initiative, whatever it is, the most important and immediate course of action to stem the tide of what’s coming — to reduce the levels of deaths and manage our adaptation to the coronavirus — is to reduce the risk of it spreading.
Bunkering down and preparing for the coronavirus is just the beginning. The coronavirus is not just a blip in the matrix. It’s a symptom of an entire system coming up against planetary boundaries. The coronavirus has erupted as a result of fossil-fuelled global industrial expansion, driving and driven by endless economic growth for its own sake, that has torn through natural systems, accelerated climate change, escalated resource depletion, entrenched inequalities, encroached human cities increasingly into animal and wildlife habitats, and massively increased the risk of disease pandemics.
And the novel coronavirus has just tipped that expanding bubble over the edge. It does look like the virus may indeed be here to stay — at least until a vaccine is created within a year to 18 months, but even then, no one has created a vaccine for a coronavirus before.
The most important thing to understand is that we don’t get through this alone. Society doesn’t get through this when each of us only cares about ourselves. The consequence of narrow self-interest, preferring business-as-usual to saving lives, is near-term global socio-economic collapse. Meanwhile, millions of lives are at stake. To that extent, millions of lives depend on the decisions each of us, particularly those in positions of power and influence.
This calls for a fundamental shift in mindset. The next quarters’ returns are not the driving issue anymore. Stock prices, oil prices, all that good stuff — these metrics are not going to save lives.
Lives are at stake.
When lives are at stake, and when you realise that you value life — life itself, for life’s sake (yes, this is called love) — you are operating to a different wavelength, one that transcends the limitations of the machine.
That doesn’t mean there are no limitations, but it means that suddenly we act not from the parameters of how an existing, broken global system limits and prevents us from saving those we love.
It means that now we don’t care about those socio-structural limits. We care about different limits. We care about natural limits which, if we respect, allow us to protect the ones we love — our fellow humans and other lifeforms.
That internal shift translates into a completely different orientation of consciousness. When we want to save the life of the one we love, we will move mountains to do so.
In this case, as we contemplate the spectre of horrendous deaths, who do we love? We love our elderly grandparents, parents, relatives and neighbours. We love our vulnerable, ill, and disabled. We love our poor, our homeless, our workers, those of us who live hand-to-mouth and can’t afford to panic-buy surplus cans of tinned food, let alone extra toilet-rolls. We love our kids, who will look up to us for guidance, protection and leadership at this time, who will follow in our footsteps in building the world to come.
And we pull out all the stops to help the ones we love. We share with them; we take care of them; we watch out for them; we check up on them; we put aside what we want; we invest ourselves in them; we sacrifice.
This is an extraordinary crisis that calls for an extraordinary human mobilisation, of which you are a potential agent and enabler, no matter where you are, what your context. And so ask yourself. At this time, what can you bring to the table? In your context, what do you offer? What is the manifestation of your love?
The potential end-result of this shift in consciousness is the capability to act beyond the broken structure of prevailing systems, and to begin to radically reshape them. The post-COVID19 system that could emerge from this crisis is one that is no longer motivated narrowly by a superfluous obsession with GDP — that measure of endless material throughout which no longer tracks with levels of happiness and well-being — but instead is inspired by the web of life.
Politicians that fail to act at this time, along with the predatory systems they preside over, will go down in history for their failure. They will be remembered for their obsession with material wealth over lives.
The question you need to ask yourself right now is, where do you stand? With the old, narrow system that is crumbling before our eyes, or a new one, weaved from the love that we hold for each other?
This article was amended on 13th March 2020 to specify that a worst-case scenario remains uncertain and is being posited for risk analysis purposes not as a forecast; to include an update on new confirmed cases; and to add some supplementary analysis of lack of scientific support for the UK government’s ‘herd immunity’ strategy.
This article was amended again on 13th March 2020 to add more material on the herd immunity strategy.
This article was amended on 14th March 2020 to provide more detail on variable fatality rates.
This article was amended on 16th March 2020 to include new material on the British government’s strategy, the herd immunity controversy, and evidence from Imperial College and a UCL Hospital doctor on the failure of the UK approach.
This article was amended on 20th March 2020 to clarify the findings of the Imperial College paper.









